COVID-19 has spurred a historic campaign for a preventive., says S.Ananthanarayanan.
To control the spread of COVID-19, we need to block the path of the virus from infected persons to susceptible persons. One way is to physically separate all people. A more practical way is that a good number of people become immune, either by recovery from the disease, or, much better, because they are protected by a vaccine. The quest for the vaccine has thus become priority.
A vaccine is a substance that gives a person the ability to prevent the virus, if it should enter the body, from affecting cells and multiplying. A first use was in 1796 by Edward Jenner when he vaccinated a 13-yr-old boy with the cowpox virus, which made the boy immune to infection by smallpox. Vaccines against a great many viral infections have been developed and many diseases are now controlled or eradicated
Since the outbreak of COVID-19, the world is racing to develop a vaccine to block SARS-CoV2, the virus that is responsible. We now have sophisticated understanding of disease and biology and over a hundred candidate vaccines are under development. The journal, Nature, carries a news feature that explains the principal routes that scientists follow.
The virus, unlike bacteria or parasites, does nothing by itself – its action is to invade and induce host cells to generate copies of the invader. Engaging the host cell blocks the cells’ own function in the body, while the virus multiplies. The virus uses two features to bring this about. The first is its outer shape or pattern, a ‘lock and-key-fit’ with the exterior of the host cell – which gives the virus entry. The second is the contents of the virus envelope –a scrap of genetic material, which, once it enters, uses the cell’s machinery to reproduce itself, and its outer shell.
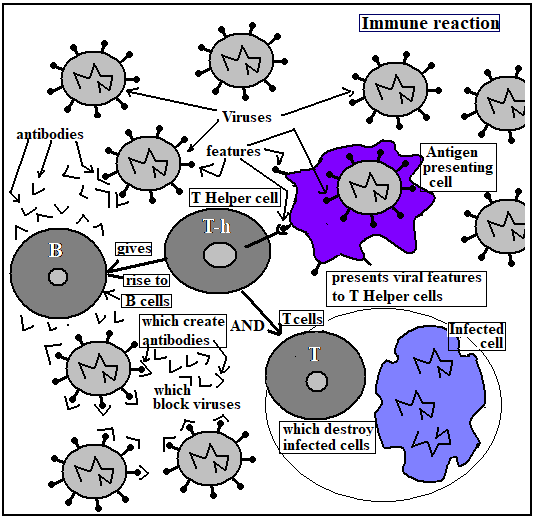
The body has a mechanism of defense against viral attack. When virus enters, cells called antigen presenting cells (APC) engulf the invader and hold out features of the virus for the attention of T-helper cells. T-helper cells activate B cells and T cells. B cells generate antibodies, or objects that attach to the virus and destroy its ability to enter a host cell. T cells go after cells that have been infected and destroy them, along with their viral contents.
The body has a mechanism of defense against viral attack. When virus enters, cells called antigen presenting cells (APC) engulf the invader and hold out features of the virus for the attention of T-helper cells. T-helper cells activate B cells and T cells. B cells generate antibodies, or objects that attach to the virus and destroy its ability to enter a host cell. T cells go after cells that have been infected and destroy them, along with their viral contents. Once these defender cells have been created, they remain in the body and if there is another infection, they act at once. A vaccine is an agent that mimics the virus to set up the B and T cells, but does not have the ability to overcome the immune system and cause disease. The present quest is to find a vaccine for COVID-19, and the Nature article describes the four main directions followed, based on viral features.
Weakened virus
One way is to use the virus itself, in a weakened or inactivated form. The virus will thus present the features that APC can use to bring about B and T cells, but the active features of the virus, to infect and multiply, are attenuated. Many existing vaccines are made in this way, vaccines for measles and polio, for instance. But this method can be dangerous and vaccines have to be carefully tested, to be sure that they are safe, before use. Sinovac Biotech in Beijing has started to test an inactivated version of SARS-CoV-2 in humans, the Nature article says.
Viral vector
Nucleic acid vaccines
A third method is not to use viruses, but to put the genetic information of the target virus directly into body cells. The cells then create the proteins and surface features of virus, and the immune system creates the antibodies to combat the virus itself, should one be encountered. This is a safe method, but it involves generation of the genetic material and then ways to insert the material into host cells. The method is still unproven and no working vaccines have been developed so far by this method. Over twenty teams are said to be working in this way to find a vaccine for COVID-19.
Protein sub-units/b>
Another step in the same direction is to insert not genetic material that would lead to proteins, but the proteins themselves. Twenty-eight teams are said to be working on this method. The focus is on the Corona virus spike protein, or the domain that binds to the receptors of target cells. Vaccines developed in this way have worked with monkeys and the SARS virus, the Nature article says. These vaccines also need accompanying substances that stimulate the immune response and may need to be administered in multiple doses.
Another version of this approach is the virus-like particle, or bodies that have no genetic content, but are shells that present just the coronavirus structure. These particles, which are challenging to manufacture, evoke strong immune response but are not infectious, as they cannot replicate.
Encouraging prospects/b>
With over a hundred groups at work on finding a vaccine, two of them have surged forward. Massachusetts based Moderna has developed a synthetic scrap of genetic material, which induces cells to produce a protein that mimics the SARS-CoV2 envelope, and has proved effective in animal trials. Oxford University researchers, with the Edward Jenner Institute for Vaccine Research, in Berkshire, England, have announced a viral vector vaccine that has protected a test batch of six rhesus monkeys, exposed to large volumes of SARS-CoV2, for over 28 days. Both groups have moved to human trials and hope to have the vaccines approved and available by September. A Swiss enterprise has started production of the Moderna vaccine and the Oxford group has tied up with seven manufacturers, including the Serum Institute of India, at Pune, which has also started production in anticipation.
This rapid progress appears to be because the Moderna vaccine is not a virus, and the vector virus chosen by the Oxford group is proven safe, as it was successful with a related coronavirus. Hence, only the efficacy of the vaccines to prevent COVID-19 in humans needs to be established.
------------------------------------------------------------------------------------------ Do respond to : response@simplescience.in-------------------------------------------